Life Changing Breathing.
The Revolutionary Magnetic Nasal Strip
Excellent 4.5 | 1,000,000+ Customers
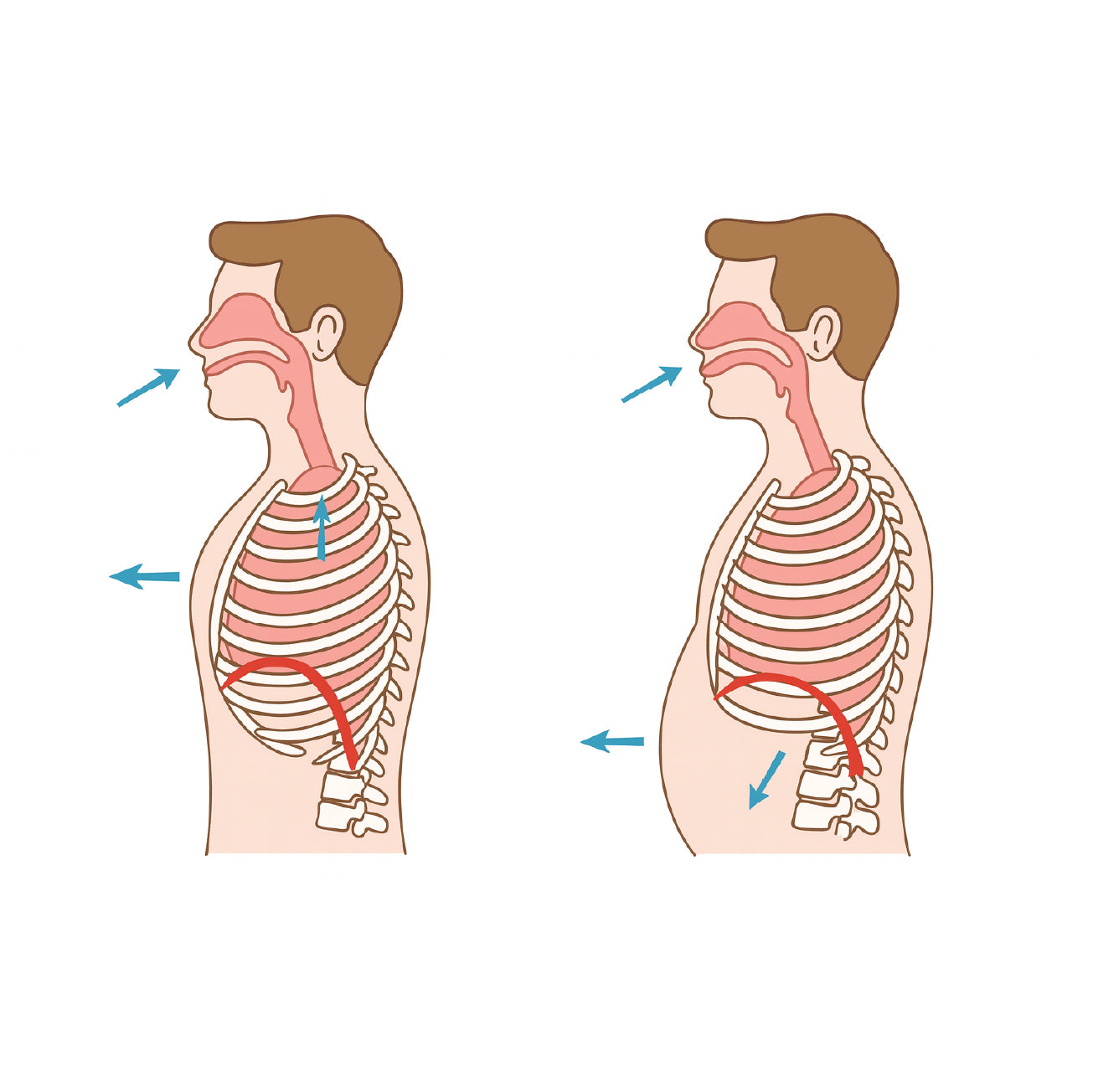
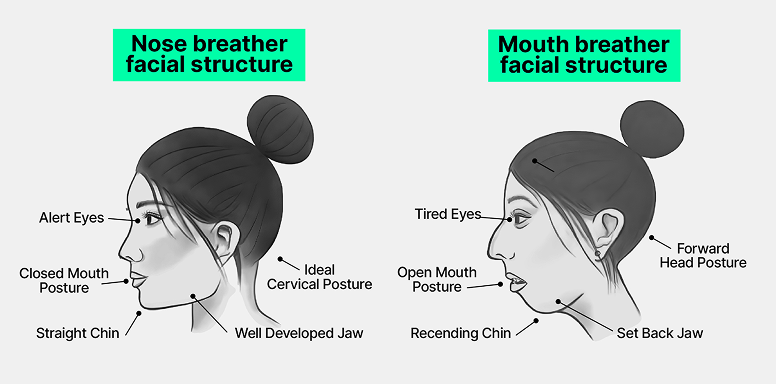
4 out of 5 people are airflow limited. Are you one of them?

Potential Health Effects of Limited Airflow

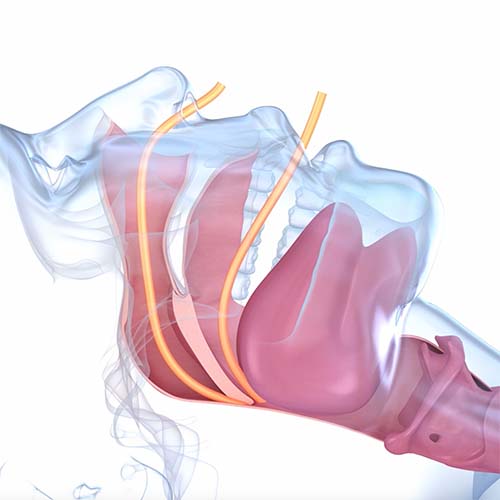
Introducing Intake Breathing.
Trusted by Millions. Backed By Research. SleepScore Labs confirms what our users experience every day, better breathing and better sleep.
-
0%Of Users Reported A Reduction In Snoring*
-
0%Of Users Reported Relief From Sinus Pressure*
-
0%Of Users Reported Deeper & More Restful Sleep*
SleepScore Labs independent study: participants with sleep tracking; over 840 nights analyzed. Read more here.
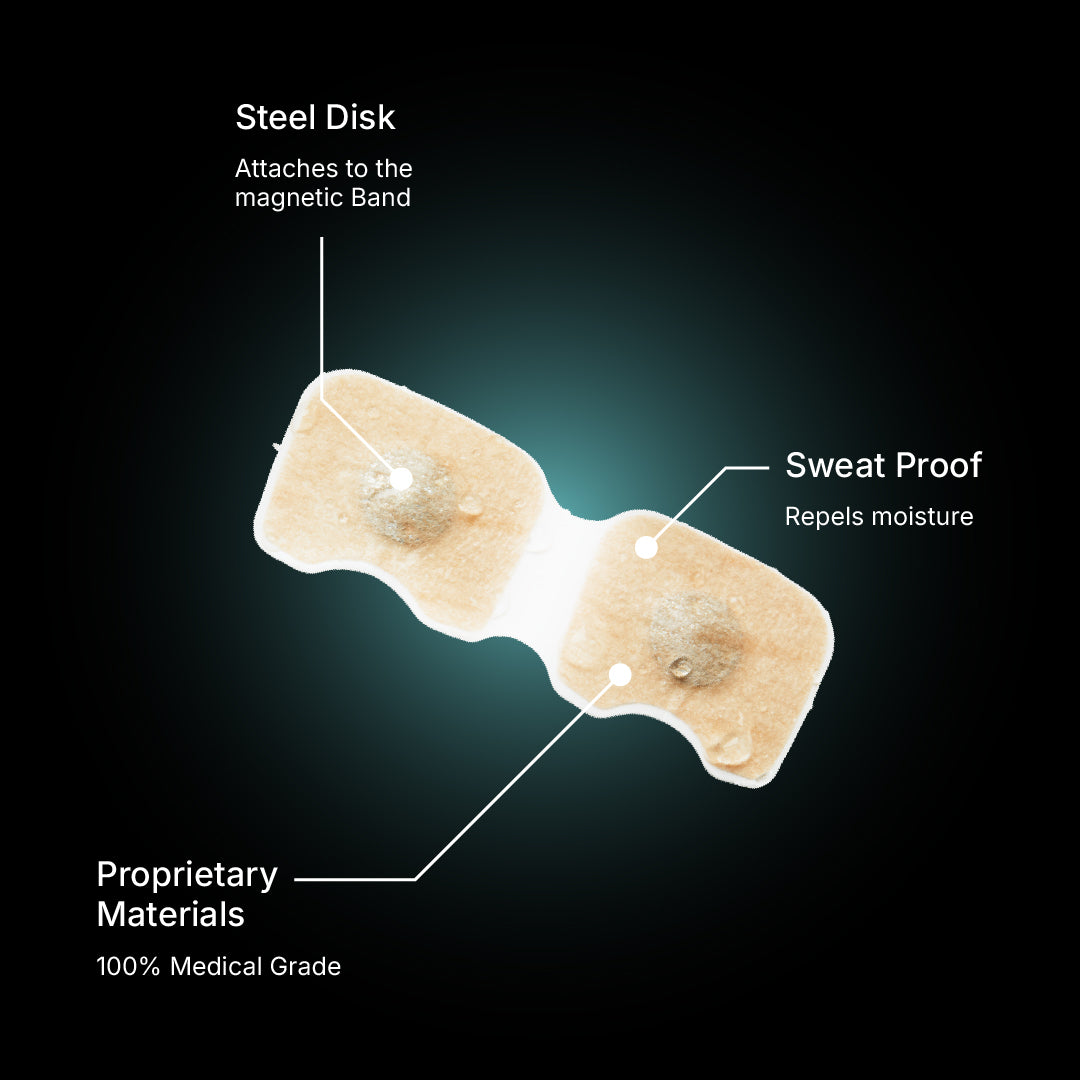
What Sets Us Apart
Intake opens your nasal passageways wider, stays put when strips slip, wicks sweat, and won’t collapse when you breathe in.

Intake

Nasal Strip
How To Use Intake
+1,000,000 Customers
FAQ
Will the tabs actually stay on overnight or when I’m sweaty?
Yes. Intake was originally designed for motocross and high-intensity athletic sports, where sweat, movement, and helmets make adhesion tough. The tabs are built to handle those conditions—and to stay on reliably through a full night’s sleep.
For best results:
- Apply to clean, dry skin (no lotions, sunscreen, or makeup).
- Clean nose with an alcohol wipe or wash with soap and water and fully dry.
- Press the tabs firmly onto your skin for 10–15 seconds.
Note: With correct placement, the tabs stay secure during workouts, runs, and all‑night wear. See our placement guide here.
With correct placement, the tabs stay secure during workouts, runs, and even all-night wear.
Will this make my nose permanently bigger?
No. Intake is an external nasal dilator. It temporarily and gently supports the nasal valve to improve airflow while worn; your nose returns to baseline when removed. Permanently changes in nasal soft tissue or cartilage come through significant force from events like surgery or trauma.
I have sensitive skin. Is the adhesive safe?
Yes. Intake pads are made with USA-made, medical-grade materials that are designed to be safe for skin contact. The adhesive is latex-free and hypoallergenic.
Will it hurt or feel uncomfortable?
No—Unlike nasal strips that pull on the bridge of your nose, Intake works differently:
- External only: Nothing goes inside your nose. The band and tabs sit gently on the outside, so there’s no internal irritation.
- No bridge pressure: Because Tabs anchor to the side of your nose, you don’t get that tugging or pulling across the bridge that many strips cause.
- Customizable fit: Intake comes in different sizes, and you can try different band sizes to change how it opens your nose. That means you control both the airflow and the comfort level.